As total ankle replacements (TARs) become more prevalent, it is essential for surgeons to be able to properly assess and address complications. Impingement of the bone or soft tissues can be a significant cause of pain after TAR. With this in mind, the authors provide salient diagnostic insights and offer perspective on conservative and surgical treatments for impingement, including open and arthroscopic repair.
Total ankle replacement (TAR) is becoming an increasingly viable treatment method for ankle arthritis. Researchers have shown that TAR is a non-inferior option to ankle arthrodesis and recent data even demonstrates a trend toward better quality of life in patients who had TAR in comparison to those who had a tibiotalar arthrodesis.1-3 Due to continued improvements in technique and implant design, there has been an increase of published data on long-term survivorship of total ankle arthroplasty.4 Despite these improvements, there are still common postoperative complications surgeons may need to address.4-6
A common but often aggravating complication is gutter pain secondary to soft tissue or bony impingement. Multiple total ankle designs reportedly cause symptomatic gutter impingement in patients post-operatively.7-11 In a 2013 study involving four different ankle replacement systems and a total of 489 procedures, Schubert and colleagues reported a seven percent incidence of symptomatic gutter impingement.12 The exact etiology behind painful malleolar gutters following TAR remains unclear but the causes seem to be complex and multifactorial in nature. Potential inciting factors include technical error, ectopic bone formation, implant design, oversized components, inadequate ligamentous balancing, undercorrection of varus/valgus deformity or component loosening.9,12-15
Pertinent Pearls In The Diagnosis Of Ankle Impingement After TAR
The diagnosis of true ankle impingement following total ankle replacement hinges on history and physical exam in combination with radiographic evidence. The pain is localized upon palpation of the medial and lateral gutters. Additionally, eliciting pain with range of motion of the ankle joint in the sagittal and coronal planes may help localize the area of impingement. Symptoms of focal gutter pain usually present three to six months following implantation as the patient increases activity.14
One then correlates the clinical findings with radiographic evidence, most commonly in the form of heterotopic ossification or abutment of the talar implant against the malleoli. Although osteophytes and ectopic bone ossification may be common following TAR, studies show that heterotopic ossification may not be associated with functional outcomes.16,17 Therefore, it is important to assess the clinical relevance of ossifications in relation to gutter pain. Heterotopic ossification may or may not coincide with synovial impingement following total ankle replacement.18
When there is uncertainty, utilizing other diagnostic tools may be beneficial. Employing computed tomography (CT) can allow surgeons to further assess the positioning of the prosthetic component and osseous impingements. Computed tomography is preferable to magnetic resonance imaging (MRI) because artifacts secondary to the metallic components may impede detailed assessment.19
Diagnostic injection with local anesthetic is another useful tool in localizing the area of pain. Due to varus or valgus deformity in the ankle joint, patients often have limited use of the posterior tibial or peroneal tendons prior to ankle replacement. After correction of the deformity, patients may commonly experience inflammation and pain in those tendons because of increased activity. A diagnostic injection within the ankle joint or tendon sheaths can help delineate whether the pain is extra-articular in nature or secondary to impingement.
Conservative Treatment For Impingement After TAR: What You Need To Know
Before considering another surgery to address gutter impingement pain following total ankle replacement, one should exhaust conservative treatments. In the early post-operative period, the patient may aggravate gutter pain from increasing activity in concurrence with post-operative inflammation. Patients may benefit from a few weeks of offloading with immobilization, rest or bracing.
Intra-articular corticosteroid injections offer another conservative treatment that can help decrease inflammation in the capsular tissues of the ankle joint. With this reduced inflammation, the reduced pressure from the thickened capsular tissue may help relieve the impingement within the medial or lateral gutters. It is important to clean the outside of the ankle prior to injection with betadine or chlorhexidine gluconate swabs so as to avoid infection to the prostheses. Also, one should avoid contacting the needle with the metallic implant as this can accelerate wear.
While it is possible that these conservative treatments may provide symptom relief, there are no current studies, to our knowledge, that assess the efficacy of these treatments for impingement symptoms following total ankle replacement.
Assessing Surgical Options For Post-TAR Ankle Impingement
Prophylactic gutter resection is not part of the surgical technique with most available TAR systems. However, in our opinion and experience, certain prostheses such as the Scandinavian Total Ankle Replacement (STAR™, Stryker) allow for gutter decompression through talar margin resection. Schuberth and colleagues found that patients who had prophylactic gutter debridement had a significantly lower incidence of secondary gutter resection than those who did not.12
Gaudot and colleagues have also identified mobile-bearing implant systems as a potential cause of malleolar gutter pain because of the excessive subluxation of the polyethylene insert.19 Thus, adopting a fixed-bearing implant design may avoid gutter impingement. Yet the evidence is unclear on whether there is a significant difference between the two types of prostheses.
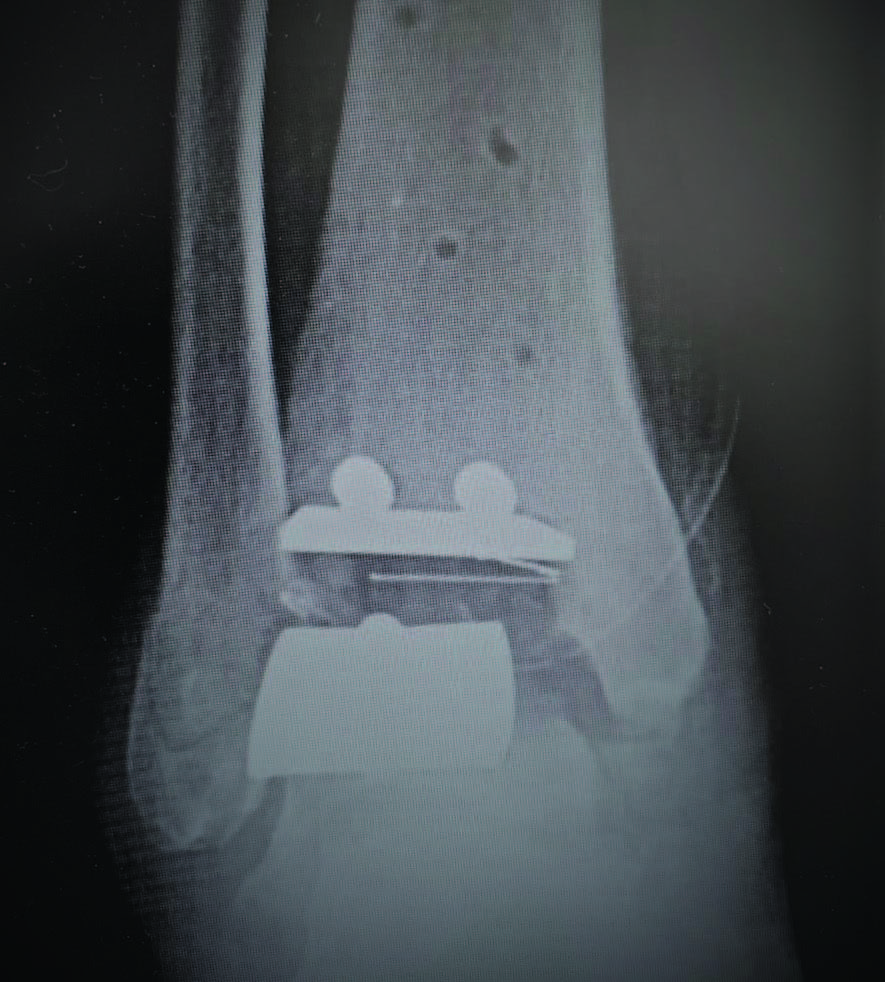
If a surgeon encounters painful malleolar gutters following TAR, it is paramount to identify the underlying cause for proper treatment. Technical error leading to malpositioning of the prosthesis is a common cause of gutter impingement pain (see top image to the left). In cases in which pain is due to malpositioned prostheses, surgeons may need to perform periprosthetic osteotomies (supramalleolar or inframalleolar) or revisional arthroplasty (see bottom image to left) to correct the deformity. The goal is to realign the joint in order to take pressure off of the symptomatic gutter. In instances of mild malposition of the prothesis, upsizing of the polyethylene insert is an option to alleviate symptoms through increased separation of the tibial and talar components.14 However, one must carefully consider the potential loss in range of motion.
Osseous overgrowth causing impingement may also attribute to aseptic loosening of the talar component.20 In such instances, a CT scan can provide a detailed assessment of the bone stock beneath the talar component. Bone cyst curettage and bone grafting may be beneficial in conjunction with resection of the osseous overgrowth. Cyst recurrence is common and complete filling of each individual cyst is often difficult.21 Therefore, revisional arthroplasty or even ankle arthrodesis may be the only solutions.
If one addresses malalignment or aseptic loosening of the prosthesis appropriately, one can perform malleolar gutter debridement through an arthroscopic or open approach.22-24 A 2.9 mm, 70-degree scope is ideal for malleolar gutter debridement. Use of an ankle distractor is the surgeon’s preference.22-24 Utilizing a combination of the shaver and grasper, the surgeon should continue to debride the gutters until there is distinct visualization of clear space between the talar bone/component and the malleoli. Once the debridement is complete, one should be able to fit the shaver within the gutters without difficulty. The advantage of arthroscopic debridement is a quicker return to activity as opposed to the open approach. However, there is significant risk of damaging the ankle components with the arthroscopic instruments due to a confined space to use the instrumentation. It is important to avoid contact to the metallic components with the shaver or burr. One must also be aware of the reflection off of the metallic component when entering the ankle joint with the shaver or burr (see top image to the right). If the surgeon is not cognizant of the orientation of the instrumentation, he or she may unintentionally damage the ankle components, and leave inflammatory debris within the ankle joint.
Debridement through an open approach allows for easier visualization and consequently a more thorough debridement of the malleolar gutters. An open approach may also decrease operating time. In instances of posterior gutter impingement secondary to ectopic ossification, an open arthrotomy is the preferred treatment option. This allows for direct visualization of the neurovascular structures that are in close proximity and difficult to avoid through an arthroscopic approach. For the open approach, one makes the incision directly over the painful gutter, taking care to protect neurovascular and tendinous structures. The surgeon can employ osteotomes and electric burrs to resect osteophytes and ectopic ossifications.
Postoperatively, patients that undergo debridement through an open ankle arthrotomy should be non-weightbearing in a posterior splint for approximately two weeks with subsequent physical therapy and progression back to regular shoes. Conversely, the patients that have arthroscopic debridement may immediately perform protected weightbearing and begin physical therapy after the first post-operative visit at one week.
Concluding Thoughts
Total ankle prostheses continue to show improvement in long-term survivorship with each evolution of implant design. Accordingly, as prostheses show increasing longevity, complications will perpetually arise following total ankle replacement. Impingement issues after total ankle replacement are a common but complex complication that require careful consideration for management. Detailed preoperative and postoperative assessments of the patient are necessary in order to properly treat symptomatic gutter impingement. Surgeons should understand the underlying causes contributing to painful impingement so they can properly address them in conjunction with gutter debridement.
Dr. Chu is a Foot and Ankle Fellow with Coordinated Health-Lehigh Valley in Bethlehem, Pa.
Dr. Brigido is the Director of the Coordinated Health-Lehigh Valley Fellowship in Bethlehem, Pa. He is a Fellow of the American College of Foot and Ankle Surgeons, and a Diplomate of the American Board of Podiatric Surgery. Dr. Brigido is board-certified in foot surgery and rearfoot/ankle surgery.
1. Haddad SL, Coetzee JC, Estok R, Fahrbach K, Banel D, Nalysnyk L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J Bone Joint Surg Am. 2007;89(9):1899-1905.
2. Saltzman CL, Mann RA, Ahrens JE, et al. Prospective controlled trial of STAR total ankle replacement versus ankle fusion: initial results. Foot Ankle Int. 2009;30(7):579-596.
3. Dalat F, Trouillet F, Fessy MH, Bourdin M, Besse JL. Comparison of quality of life following total ankle arthroplasty and ankle arthrodesis: retrospective study of 54 cases. Orthop Traumatol Surg Res. 2014;100(7):761-766.
4. Clough T, Bodo K, Majeed H, Davenport J, Karski M. Survivorship and long-term outcome of a consecutive series of 200 Scandinavian Total Ankle Replacement (STAR) implants. Bone Joint J. 2019;101-B(1):47-54.
5. Rippstein PF, Huber M, Naal FD. Management of specific complications related to total ankle arthroplasty. Foot Ankle Clin N Am. 2012;17:707-717.
6. Jonck JH, Myerson MS. Revision total ankle replacement. Foot Ankle Clin N Am. 2012;17(4):687-706.
7. Koivu H, Kohonen I, Mattila K, Loyttyniemi E, Tiusanen H. Long-term results of Scandinavian Total Ankle Replacement. Foot Ankle Int. 2017;38(7):723-731.
8. Cerrato R, Myerson MS. Total ankle replacement: the Agility LP prosthesis. Foot Ankle Clin. 2008;13(3):485-494.
9. Rippstein PF, Huber M, Coetzee JC, Naal FD. Total ankle replacement with use of a new three-component implant. J Bone Joint Surg Am. 2011;93(15):1426-1435.
10. Harston A, Lazarides AL, Adams SB Jr, DeOrio JK, Easley ME, Nunley JA 2nd. Midterm outcomes of a fixed-bearing total ankle arthroplasty with deformity analysis. Foot Ankle Int. 2017;38(12):1295-1300.
11. Nunley JA, Adams SB, Easley ME, DeOrio JK. Prospective randomized trial comparing mobile-bearing and fixed-bearing total ankle replacement. Foot Ankle Int. 2019;40(11):1239- 1248.
12. Schuberth JM, Babu NS, Richey JM, Christensen JC. Gutter impingement after total ankle arthroplasty. Foot Ankle Int. 2013;34(3):329- 337.
13. Gross CE, Adams SB, Easley M, Nunley JA 2nd, DeOrio JK. Surgical treatment of bony and soft-tissue impingement in total ankle arthroplasty. Foot Ankle Spec. 2017;10(1):37-42.
14. Schuberth JM, Wood DA, Christensen JC. Gutter impingement in total ankle arthroplasty. Foot Ankle Spec. 2016;9(2):145-158.
15. Krause FG, Windolf M, Bora B, Penner MJ, Wing KJ, Younger ASE. Impact of complications in total ankle replacement and ankle arthrodesis analyzed with a validated outcome measurement. J Bone Joint Surg Am. 2011;93(9):830-839.
16. Choi WJ, Lee JW. Heterotopic ossification after total ankle arthroplasty. J Bone Joint Surg Br. 2011;93(11):1508-1512.
17. Bemenderfer TB, Davis WH, Anderson RB, et al. Heterotopic ossification in total ankle arthroplasty: case series and systematic review. J Foot Ankle Surg. 2020. [Epub ahead of print] Available at: https://www.jfas.org/article/ S1067-2516(19)30452-1/fulltext . Published January 16, 2020. Accessed April 14, 2020.
18. Besse J, Bevernage BD, Leemrijse T. Revision of total ankle replacements. Tech Foot Ankle Surg. 2011;10(4):176-188.
19. Gaudot F, Colombier J-A, Bonnin M, Judet T. A controlled, comparative study of a fixed-bearing versus mobile-bearing ankle arthroplasty. Foot Ankle Int. 2014;35(2):131-140.
20. Younger A, Penner M, Wing K. Mobile-bearing total ankle arthroplasty. Foot Ankle Clin. 2008;13(3):496-508.
21. Besse J-L, Lienhart C, Fessy M-H. Outcomes following cyst curettage and bone grafting for the management of periprosthetic cystic evolution after AES total ankle replacement. Clin Podiatr Med Surg. 2013;30(2):157-170.
22. Richardson AB, DeOrio JK, Parekh SG. Arthroscopic debridement: effective treatment for impingement after total ankle arthroplasty. Curr Rev Musculoskelet Med. 2012;5(2)171-175.
23. Shirzad K, Viens NA, DeOrio JK. Arthroscopic treatment of impingement after total ankle arthroplasty: technique tip. Foot Ankle Int. 2011;32(7):727-729.
24. Kim BS, Choi WJ, Kim J, Lee JW. Residual pain due to soft-tissue impingement after uncomplicated total ankle replacement. Bone Joint J. 2013;95-B(3):378-383.